Too low for Zero - the Elton John AIDS Foundation SIB
Sam Magne, Knowledge and Learning Manager at The National Lottery Community Fund (the Fund), reflects on Ecorys/ATQ’s first in-depth report on Elton John AIDS Foundation’s (The Foundation’s) Social Impact Bond (SIB) funded by the Fund’s Commissioning Better Outcomes (CBO) programme. Sam asks whether, in a plot twist on the core SIB tune, the Elton John AIDS Foundation has a trick or two to teach fellow Foundations and grant-makers about leveraging system-change.
Sam Magne, Knowledge and Learning Manager at The National Lottery Community Fund (the Fund), reflects on Ecorys/ATQ’s first in-depth report on Elton John AIDS Foundation’s (The Foundation’s) Social Impact Bond (SIB) funded by the Fund’s Commissioning Better Outcomes (CBO) programme. Sam asks whether, in a plot twist on the core SIB tune, the Elton John AIDS Foundation has a trick or two to teach fellow Foundations and grant-makers about leveraging system-change.
Double-back to this time the other side of the Millennium and the global issue breaking onto the epidemiological timeline is AIDS. Four decades later, huge strides have been made in reducing transmission and changing outcomes for people who contract HIV, through retroviral treatment and community engagement and support.
These advances create the possibility of the ultimate epidemiological ambition being achieved - eradication of the disease by reducing transmission to zero. And yet, the keys to realising the goal - comprehensive testing to pick up cases early in areas where rates of under-detection and infection are highest, together with personalised support alongside retroviral therapy for those diagnosed with HIV - have often not been grasped by health practitioners.
The Foundation’s Zero HIV SIB aims to change that. The initiative builds on The Foundation’s ethnographic research and pilot projects. These studies revealed that with all the pressures that health practitioners work under, awareness of localised prevalence was low, as were the capacity and capabilities of medics to start out-of-context conversations with patients in the general population about opting-in to testing. The Public Health system’s default approach is to pay practitioners per test conducted but, psychologically speaking, the price set is too low to trigger those difficult conversations.
The Foundation concluded that health services’ impetus to test had to be dialled up far enough – motivationally and financially - to overcome the daily inhibitors and stresses of general practice and outpatient services. So The Foundation came up with a plan to switch things around, by implementing an opt-out approach to testing for HIV in key geographies, and incentivising health practitioners to test and follow up with treatment and support. Payment would not be made for tests conducted, but instead for positive results detected and, for successfully engaging patients in sustained treatment.
That’s where the idea for a SIB came in – as a results-based payment device with a big enough price-tag to draw attention to producing clinical results. SIBs typically involve a payment by results (PbR) contract between a commissioner and service providers, while the upfront costs of delivering interventions are covered by social investors. There are many variations on this core SIB theme tune, but The Foundation’s is particularly inventive.
In their Zero HIV SIB, the Fund provides a proportion of the outcomes payments, but unusually it’s The Foundation’s - a grant-making organisation – and not a public body that’s the principle commissioner. Local Authorities are involved (see below*) but only Lambeth Council has directly provided financial support. Ideally, public organisations would fully fund the Social Impact Bond’s outcomes, but HIV testing and treatment is one of the early-action public services which falls foul of the ‘wrong pocket’ problem: the body that would like (or is tasked) to find a way to pay for the preventative work (in this case Public Health, which is now part of local government), doesn’t stand to gain the savings it generates (in this case, it’s the NHS’s secondary care services which would). To break this stand-off, The Foundation has intervened, using its own charitable funds to pay the lion’s share of the outcomes, with a view to demonstrating to both Public Health and the NHS that the opt-out model with the outcomes-based payment regime is a game-changer.
The Foundation’s intervention also includes a complex arrangement in which The Foundation straps the boroughs in as co-commissioners but then reimburses them*. The Foundation argues this at least captures Public Health’s cooperation as allies in observing the model’s effects and in persuading the NHS to paying for it in the future. In addition, The Foundation also hopes the learning from the model can be applied internationally, where they can see it working as a Development Impact Bond.
In this UK SIB the overall costs that stand to be avoided are impressive from an NHS accountancy angle. But it’s the nuance of how the cash is sourced and deployed that gives the SIB traction through its supply chain layers.
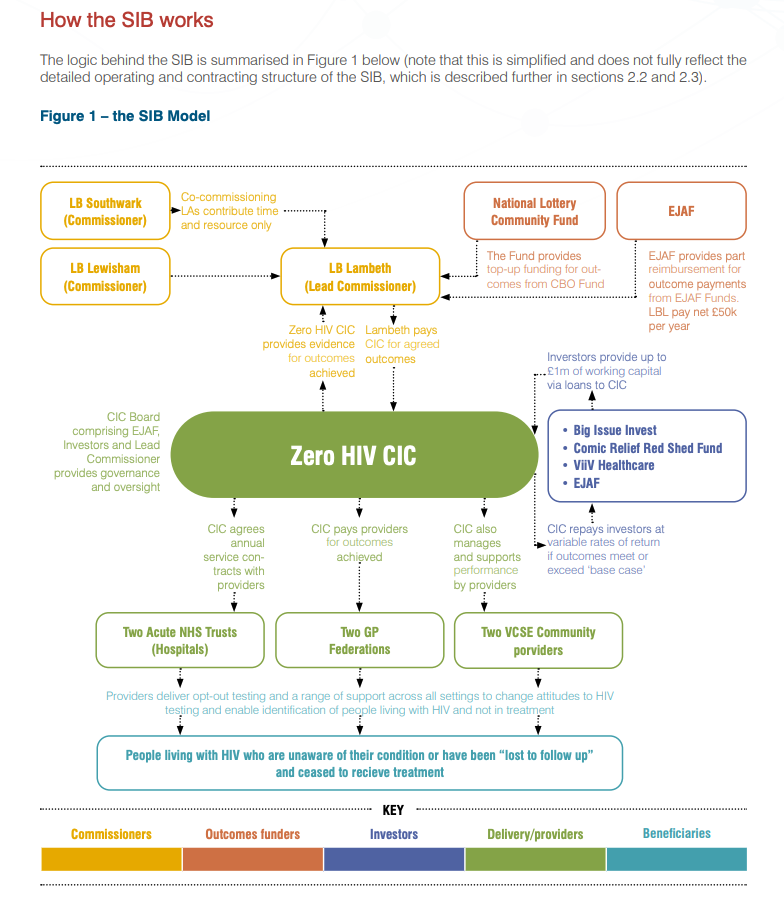
The deal involves an up-front payment – like a minimum-outcomes order – to GP Federations, Hospital Trusts and third sector community health settings to get the ball rolling, followed up by standard PbR. This is passed down to A&E services, clinics and labs as Fee-for-Service payments and to GPs as an agreed share. This is packaged up with performance data, support from management at the Trusts and a GP HIV champion appointed by the Federations, to help push the PbR influence down the system. Meanwhile, the up-front sum that primes the cashflow, comes from a risk-tiered investment stack from ViiV Healthcare (a private investor), Comic Relief, Big Issue Invest and the Foundation - with BII lending from its reserves rather than drawing on its investment funds and, with The Foundation providing first-loss if outcomes are not achieved.
It’s highly unusual for the same body to work at both the commissioning and investing ends of a SIB. As both first-loss investor and commissioner, The Foundation will either carry the costs of failure, or success. ATQ point out there could be more straightforward ways to work. It would be much simpler for The Foundation to offer providers a binary contract, involving an up-front minimum-order grant and then straight PbR. However, The Foundation argue that due to the size of the up-front payments, plus the costs of setting up their Zero HIV CIC as a data and performance manager, they needed their investment pool to share the PbR working capital load - and hence a SIB.
Their system-change ambition is impressive and The Foundation may well teach us a fascinating trick or two. But this SIB involves a finely tuned arrangement with several cascades of influence and cash-flow that must harmonize to achieve results. ATQ’s next visit will report on how that tuning performs, and whether it can hit the sweet spot that will bring HIV to Zero.
 Samantha Magne
Samantha Magne